From my America Out Loud Pulse podcast with Dr. Dustin Sulak – https://www.americaoutloud.news/the-highs-and-lows-of-medical-cannabis/
Pot, Mary Jane, weed, grass, and reefer are among the many names for marijuana. Marijuana is one strain of cannabis, the plant species that includes hemp. Hemp contains low levels of the psychoactive compound delta-9-tetrahydrocannabinol (THC) and marijuana has high levels. Another active compound in cannabis is cannabidiol (CBD) and it is non-psychoactive. Any Baby Boomers who indulged can confirm that the amount of THC in marijuana has increased over the last 25 years. In the mid-1990s, the average THC content of confiscated weed was roughly 4 percent. By 2014, it was about 12 percent, with a few strains of pot containing THC levels as high as 37 percent.
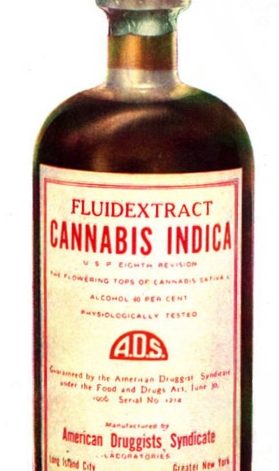
Cannabis was a key crop of the early American colonists. Indeed, one of our first president, George Washington’s main crops was hemp. In fact, the Virginia, Massachusetts, and Connecticut colonies were required to grow it. Hemp was used for fabric and rope. It wasn’t until the mid 1800s that cannabis was sold in doctors’ offices and pharmacies for medicinal purposes in the United States, mainly for stomach problems.
Cannabis had been used medicinally and recreationally for thousands of years, with artifacts from China suggesting it was used for malaria, poor memory, gout, and rheumatism. Immigrants from Mexico during the Mexican Revolution in the early 1900 were primarily responsible for the start of recreational use in the U.S. Unfortunately, during the Depression and the Prohibition era, the focus shifted to outlawing cannabis as an evil brought here by Mexican immigrants. By 1931, 29 states had outlawed cannabis. The Marijuana Tax Act of 1937 made selling, possessing or transferring hemp products for anything but industrial use a crime. The first person to violate the Act was sentenced to 4 years of hard labor.
Although the Controlled Substances Act of 1970 repealed the Marijuana Tax Act, the law made marijuana a Schedule I drug, meaning it had no medical use and the potential for addiction. This is the category that includes heroin, ecstasy, and LSD! But things began to change when California’s Compassionate Use Act of 1996 legalized marijuana for medical use by chronically ill persons. Today medical marijuana is legal in all but 11 states, although it remains illegal under federal law.
Recreational marijuana has been gradually moving from the culprit in “Reefer Madness” to a mainstream indulgence. However, many fear complete legalization as cannabis – thanks to its narcotic Schedule I status – has not had the research it deserves. (Fortunately, the Department of Health and Human Services has recommended to the Drug Enforcement Administration that the cannabis be downgraded to the class of drugs with more safety and lower potential for abuse.)
Many doctors are not familiar with the types of cannabis and the various uses. It can sometimes help patients when other more mainstream medications and treatments have failed.
My guest today is an integrative medicine physician and a highly regarded national expert in the use cannabis.
Dr. Sulak’s website: Healer.com; HealerCBD.com
Bio
Dustin Sulak, D.O. is a renowned integrative medicine physician based in Maine, whose practice balances the principles of osteopathy, mind-body medicine, spirituality in healthcare, and medical cannabis. Dr. Sulak educates medical providers and patients on its clinical use. Dr. Sulak excels in the treatment of patients with conditions that have not responded well to conventional treatment. Dr. Sulak received undergraduate degrees in nutrition science and biology from Indiana University, a doctorate of osteopathy from the Arizona College of Osteopathic Medicine, and completed an internship at Maine-Dartmouth Family Medicine Residency.